More Information
Submitted: October 04, 2024 | Approved: October 14, 2024 | Published: October 15, 2024
How to cite this article: Romuald DS, Siransy KL, Koffi N, Yeboah RO, Nguessan EK, Adou HA, et al. Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization). Arch Asthma Allergy Immunol. 2024; 8: 007-012. Available from: https://doi.org/10.29328/journal.aaai.1001035.
DOI: 10.29328/journal.aaai.1001035
Copyright License: © 2024 Romuald DS, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Latex sensitization; Impact on asthma control; Impact on rhinitis control
Impact of Latex Sensitization on Asthma and Rhinitis Progression: A Study at Abidjan-Cocody University Hospital - Côte d’Ivoire (Progression of Asthma and Rhinitis related to Latex Sensitization)
Dasse Sery Romuald1,2*, KL Siransy2, N Koffi1, RO Yeboah1,2, EK Nguessan1, HA Adou1,2, VP Goran-Kouacou1,2, AU Assi1,2, JY Seri1,2, S Moussa2, D Oura2, CL Memel2, H Koya2 and E Atoukoula2
1Department of Immunology and Allergology, University Hospital Centre of Cocody, Abidjan BP V 13, Côte d’Ivoire
2Laboratory of Immunology, Medical Teaching and Reaserch Unit of Félix Houphouet BOIGNY University, BP V 166 Abidjan, Côte d’Ivoire
*Address for Correspondence: Dasse Sery Romuald, Medical Doctor and PhD, Department of Immunology and Allergology, University Hospital Centre of Cocody, Laboratory of Immunology, Medical Teaching and Reaserch Unit of Félix Houphouet BOIGNY University, BP V 166 Abidjan, Côte d’Ivoire, Email: [email protected]
Background: The frequency of latex allergy is increasing, posing a major health problem. This increase is related to the widespread use of latex materials and cross-reactions between latex proteins and certain foods. This cross-reactivity makes latex avoidance difficult, and latex sensitization is likely to worsen atopic conditions.
Objective: The authors evaluated the role of latex sensitization in the poor control of asthma and rhinitis.
Methodology: An analytical cross-sectional study was conducted on 1860 patients of all ages and genders, followed up for allergic asthma and rhinitis since March 2012 in the Immuno-Allergology Unit of the Cocody University Hospital in Abidjan. Prick tests with native extracts and the European standard battery were performed to identify allergenic sensitization. The impact of latex sensitization on asthma and rhinitis control was assessed by calculating odds ratios.
Results: A high frequency of latex sensitization was associated with asthma and rhinitis. The risks of poor control were related to monosensitization to latex and were even higher in the context of polysensitization.
Conclusion: The impact of latex sensitization on the progression of asthma and rhinitis has been well demonstrated. It is recommended to integrate the latex sensitization status into the therapeutic management strategy of these two pathologies.
The sap of the Hevea brasiliensis tree, also called latex, is natural rubber. It is a source of ubiquitous allergenic proteins which are included in the composition of many currently used products [1-3].
These proteins are frequently associated with allergic reactions much more in the form of type I hypersensitivity IgE-mediated than type IV [4].
Latex allergy has significantly increased worldwide, likely due to widespread latex product use and other factors since the first cases were described in Europe in 1927 [2,3,5-8].
Despite efforts to mitigate the consequences of latex allergy, it has become a major health problem [4].
In developing countries context, the lack of epidemiological data is associated with the low level of education in the general population, poorly informed about this health problem. Therapeutic management is more difficult since latex is the cause of the cross allergy [9,10].
In Côte d’Ivoire, the use of latex-based products and plant foods clinical cross-reactivity with latex [1,4,9,10], could make eviction procedure extremely difficult. In such a context, allergenic sensitization to latex could have an impact on the evolution of atopic pathology. This study aimed to evaluate the role of latex sensitization in the worsening of asthma and rhinitis.
The authors performed a cross-sectional study with the analytical aim of 1860 patients aged from 2 to 68 years old. Without sex consideration, patients were followed up from March 2012 to February 2024, in the Immuno-Allergology Unit of Cocody University Hospital, for allergic manifestations management.
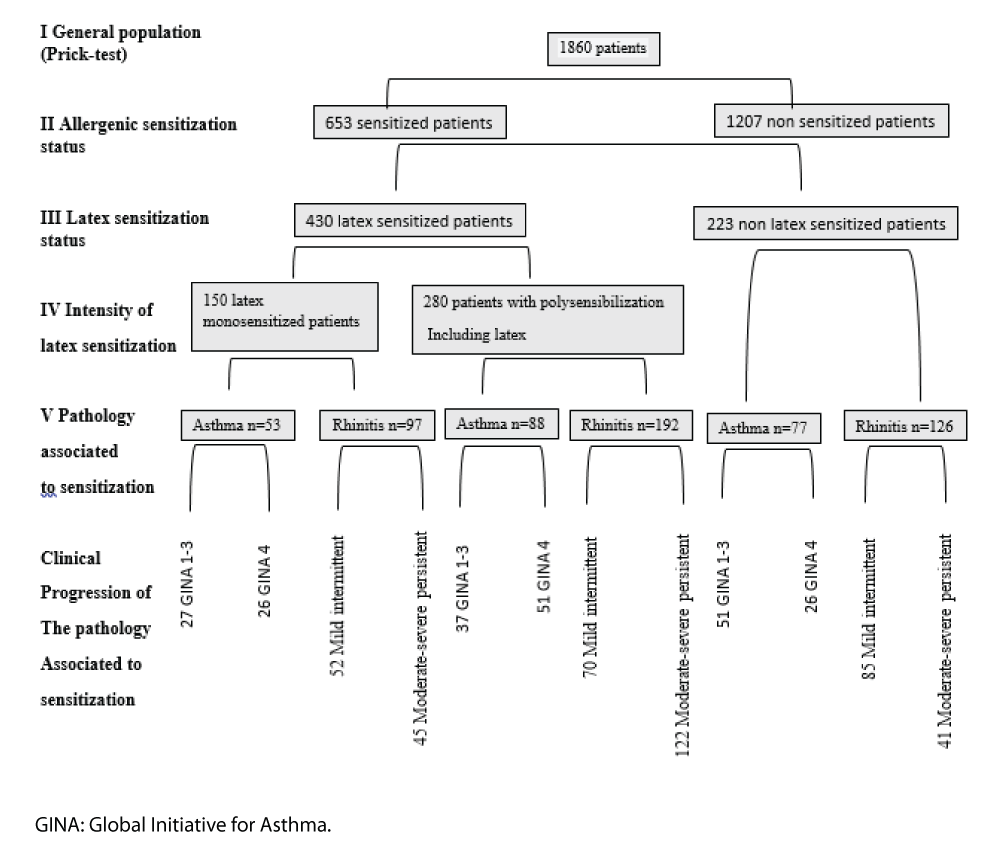
Clinical examination and Prick tests using either native extracts or the European standard battery have been performed to classify the patients. As it is shown in the flow chart (Figure 1), patients were divided into a “sensitized group (latex-mono and poly-sensitized persons)” and a “non-sensitized group”.
Figure 1: Flowchart depicting the various stages of patient selection.
The flowchart in Figure 1 presents the successive steps in patient selection. In a study of 1,860 patients, prick tests revealed that 653 were sensitized to allergens, while 1,207 were not. Among the sensitized patients, 430 reacted to latex, and 223 to other allergens. The 430 latex-reactive patients were further divided based on the intensity of sensitization: 150 were monosensitized to latex, and 280 were polysensitized to various allergens, including latex. These patients were then categorized by pathology: 53 asthma patients were monosensitized to latex, while 88 were polysensitized. Similarly, 97 rhinitis patients were monosensitized, and 192 were polysensitized. Among the non-sensitized group, 77 had asthma, and 126 had rhinitis. Finally, all patients were classified by severity: asthma patients were staged according to GINA guidelines (stages 1-3), and rhinitis patients were classified per ARIA (Allergic Rhinitis and its Impact on Asthma) guidelines into Mild Intermittent and Moderate-Severe Persistent stages.
On the other hand, asthma patients were classified into the “Asthma Group,” subdivided according to the GINA guidelines [11] into “stages 1-3” and “stages 4-5”. Rhinitis patients, called “Rhinitis Group,” were subdivided according to ARIA guidelines [12] into “mild intermittent” and “moderate-severe persistent.” The impact of latex sensitization on the control of these two affections was assessed by calculating the odds ratio.
Frequency of allergenic sensitization in the general population followed up.
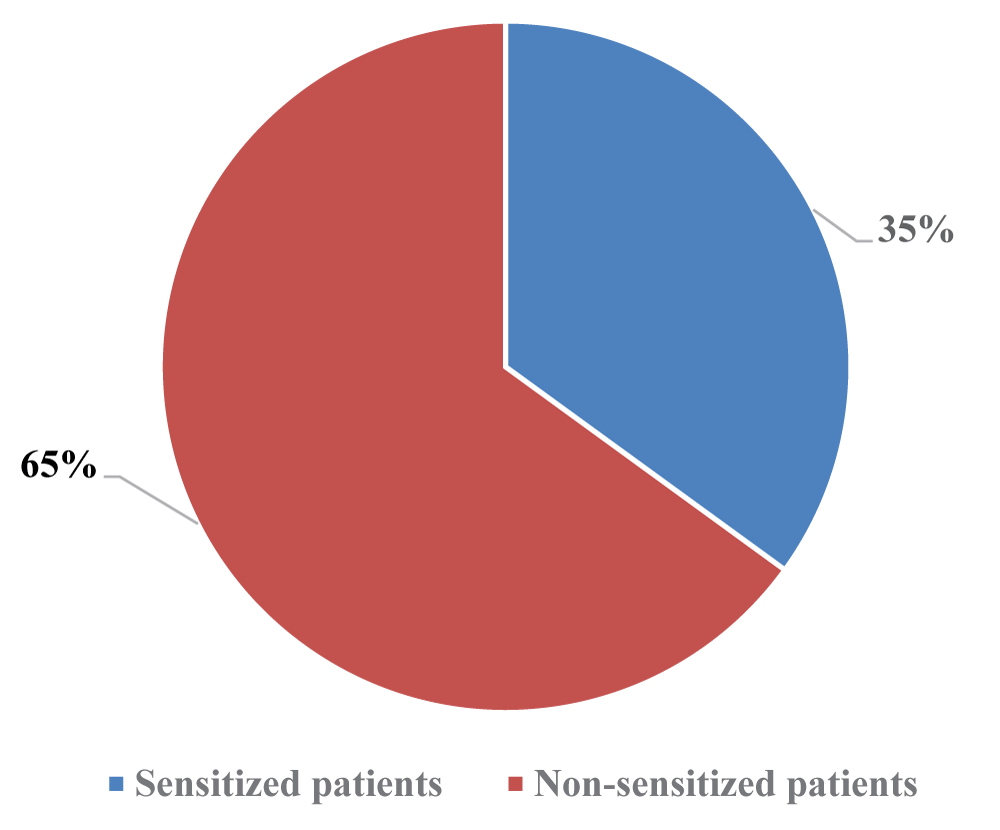
The pie chart in Figure 2 illustrates the distribution of allergenic sensitization status among patients monitored in the Allergy Unit. Out of 1860 patients, 653 (35%, highlighted in blue) were sensitized to various allergens, including latex.
Figure 2: Distribution of the patient population monitored in the Immuno-Allergology Unit, based on allergenic sensitization status.
Latex sensitization
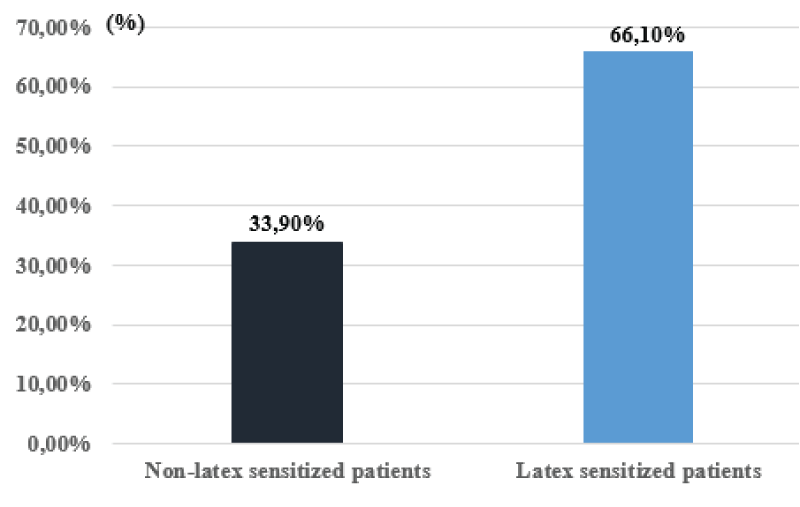
Of the 653 sensitized patients, 430 (66,10%) are sensitized to latex. Additionally, 33,90% (n = 223) exhibit sensitization to allergens other than latex. On one hand, a total of 141 patients suffering exclusively from asthma showed either monosensitization to latex (n = 53) or polysensitization to latex-associated allergens (n = 88). On the other hand, 289 patients suffering exclusively from allergic rhinitis exhibit monosensitization to latex (n = 97) or polysensitization to latex-associated allergens (n = 192).
Impact of latex sensitization
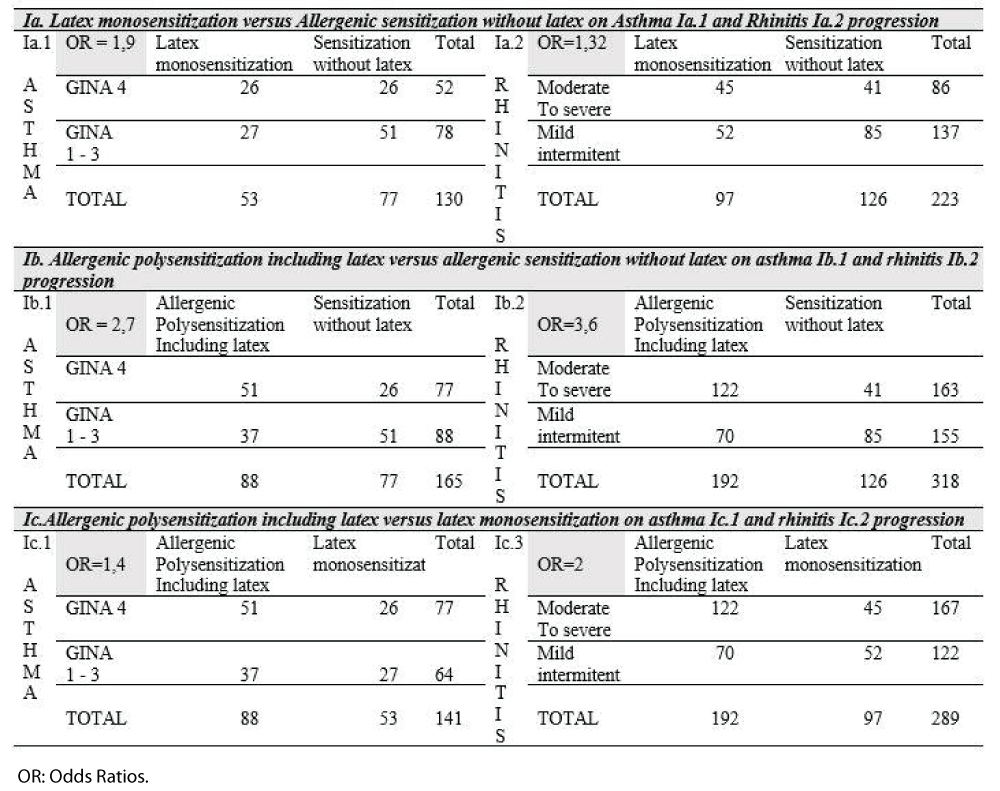
The text outlines the impact of latex-allergenic sensitization on asthma and rhinitis progression. Table 1 summarizes these effects. Table 1a-1c compares monosensitization to latex with allergenic sensitization without latex in worsening asthma and rhinitis. Table Ia1 details the risk of asthma progression from grades 1-3 to grade 4 per GINA guidelines, while Table 1a2 covers the risk of rhinitis progression from mild intermittent to moderate severe per ARIA guidelines. Table 1b assesses polysensitization, including latex, against sensitization without latex, with similar evaluations in Tables 1b1 and 1b2 Lastly, Table 1c(1-2) compares allergenic polysensitization involving latex to monosensitization. Odds ratios indicate that monosensitization to latex increases the risk of asthma (1.9) and rhinitis (1.32) progression. Polysensitization, including latex, significantly raises the risk, with asthma at 2.7 and rhinitis at 3.6. Polysensitization also affects clinical progression, with odds ratios of 1.4 for asthma and 2 for rhinitis.
Table 1: Impact of latex sensitization on the progression of asthma and rhinitis.
Prevalence of allergies and allergenic sensitization
The prevalence of allergic diseases is increasing in developed countries [13-15]. Concerning allergenic sensitization, its prevalence is just under 55% among adults in the USA [16].
In Sub-Saharan Africa, Agodokpessi, et al. in Benin, and NGOM, et al. in Ivory Coast both noted a high frequency of sensitization. The grouped results regarding sensitization to aeroallergens among patients suffering from asthma and rhinitis in the two countries are indicated below: mites (99.6%), cockroaches (71.3%), Alternaria alternata (71%), dog and cat (68%) [17,18].
In our series, out of 1860 patients, 653 (35%, highlighted in blue slice – Figure 2) are sensitized to allergens such as mites, crustaceans, fruits, and latex. Latex sensitization: Latex sensitization was higher (66%) among sensitized patients in the study population (Figure 3). This high frequency is related to the widespread and increasing use of latex-based products.
Figure 3: Distribution of patients based on latex sensitization.
This argument is further supported by numerous other factors. Indeed, chronic exposure to latex is a contributing factor to sensitization, as reported by West R W [19]. In our series, approximately 15% of patients work in professions known to be at risk (healthcare personnel) [19], rubber field workers) [20], where exposure to latex products (gloves) and the sap of Hevea brasiliensis is constant. Additionally, Ivorians are reputed consumers of bananas and avocados, two fruits with allergens that cross-react with latex.
Impact of latex sensitization on the progression of asthma and rhinitis
In the pathophysiology of allergy, the sensitization phase plays a crucial role in specific reactivities. Repeated exposure to the allergen often raises the hypothesis of the impact that this sensitization may have on the clinical progression of allergic diseases. Asthma specialists frequently report other predictive factors of severity beyond allergic sensitization. These include passive smoking, early onset of wheezing, the number of hospitalizations due to exacerbations, and the presence of aggravating factors [21-23], as well as comorbidities [24].
Regarding allergic sensitization, more and more authors are identifying it as a factor influencing the severity of respiratory atopic diseases. Indeed, it has been reported that polysensitization, particularly to dust mites, strongly influences the worsening of allergic rhinitis and conjunctivitis in children [25]. The predominant role of indoor allergen sensitization has also been well documented in the worsening of asthma in children, the majority of whom are sensitized to indoor allergens [26].
The phenomenon of continuous exposure to allergens certainly plays a key role, as was observed during the COVID-19 pandemic with periods of lockdown [27]. This is particularly noticeable with recurrent exposure to latex in high-risk professions, such as healthcare workers and those involved in natural rubber production [1]. Furthermore, the specific characteristic of latex lies in its cross-reactivity with food allergens, which gives this allergen a ubiquitous nature, simulating recurrent contact with the patient. In a 2002 systematic review, James Fish highlighted that occupational exposure to Natural Rubber Latex (NRL) in healthcare workers can cause rhinitis and conjunctivitis symptoms. However, the risk and prevalence of NRL-induced asthma remain low due to the large size of the allergens, which prevents them from easily entering the lower airways [28].
While the link between latex sensitization and allergic pathology is reported how this sensitization may impact the progression of asthma and rhinitis remains to be demonstrated.
The authors have shown that progression to stage 4 GINA guidelines is influenced by monosensitization to latex despite good adherence to treatment (Table 1).
The risk is even higher when latex sensitization is associated with other allergens. The same observation is reported in the progression of allergic rhinitis, where the transition from intermittent to moderate-severe persistent stages was influenced by strong latex sensitization.
Continuous contact with latex-based products is the cause. In Côte d’Ivoire, despite the decree banning the use of plastic bags [29,30], there is a high usage of these products by the general population. Indeed, the population seems to be poorly informed about the consequences of allergic pathology. The impact on the occurrence and worsening of allergic manifestations to latex is not sufficiently highlighted. This is partly due to the lack of epidemiological data in this resource-limited country context.
Latex allergy is due to a strong allergenic sensitization associated with manifestations of asthma and rhinitis. It is a major public health issue. Sensitization to latex is well demonstrated as a risk factor for the worsening of these two pathologies. The role of latex in cross-allergies is certainly the cause of the difficulty in implementing avoidance procedures. Therefore, data on latex sensitization should be integrated into the management strategy for asthma and rhinitis.
Highlights of this article
- The increasing prevalence of latex sensitization complicates latex avoidance.
- Latex sensitization strongly impacts asthma and rhinitis control, especially in polysensitization.
- Incorporate latex sensitization status into asthma and rhinitis management strategies.
We thank Dr. Nguessan Emmanuel for his daily involvement in the reception and performance of the Prick tests.
Ethical considerations
All patients gave their informed consentment for the publication of anonymous data and the study benefited from the agreement of the Medical and Scientific Department of the University Hospital of Cocody (CHU Cocody under the N°.007-12/MSHPCMU/CHU-C/DMS/cm.
Author contribution
Dasse SR designed the study; Dasse SR, Siransy KL, Yeboah OR, and Adou AH acquired, analyzed, and interpreted data; Dasse SR and Nguessan K drafted the article. Adou AH, Kouacou Amah V P, Assi A U A, Siransy KL, Séri YJ, Moussa S, Oura D, Memel CL, Koya H, Attoukoula LA revised it critically for important intellectual content. All authors approved the final version to be submitted and agreed to be accountable for all aspects of the work.
- Cabañes N, Igea JM, de la Hoz B. Latex allergy: position paper. J Investig Allergol Clin Immunol. 2012;22(5):313-330. Available from: https://pubmed.ncbi.nlm.nih.gov/23101306/
- Walls RS. Latex allergy: a real problem. Med J Aust. 1996;164:707-708. Available from:https://doi.org/10.5694/j.1326-5377.1996.tb122264.x
- Blanco Guerra C, Quirce Gancedo S, de la Hoz Caballer B, Nieto Garcia A, Tabar Purroy A. Hypersensitivity reactions to rubber tree latex. In: Allergology Treatise. Pelaez D, Davila E, editors. Ergon; 2007;1657-1680.
- Parisi CAS, Kelly KJ, Ansotegui IJ, Gonzalez-Díaz SN, Bilò MB, Cardona V, et al. Update on latex allergy: new insights into an old problem. World Allergy Organ J. 2021;14:100569. Available from: https://doi.org/10.1016/j.waojou.2021.100569
- Purroy A. Hypersensitivity reactions to rubber tree latex. In: Allergology Treatise. Pelaez D, Davila E, editors. Ergon; 2007;1657-1680.
- Barber Hernandez D, Lombardero Vega M. Allergenic composition of latex. In: Alergia a látex. Mra Ediciones; 2002;13-25.
- Stern G. Hypersensitivity to rubber as a cause of urticaria and Quincke's edema. Klin weekly magazine. 1927;6:1096-1097.
- Nutter AF. Contact urticaria to rubber. Br J Dermatol. 1979;101:597-598. Available from: https://doi.org/10.1111/j.1365-2133.1979.tb11893.x
- Carrillo T, Cuevas M, Muñoz T, Hinojosa M, Moneo I. Contact urticaria and rhinitis from latex surgical gloves. Contact Dermatitis. 1986 Aug;15(2):69-72. Available from: https://doi.org/10.1111/j.1600-0536.1986.tb01279.x
- Ebo DG, Hagendorens MM, De Knop KJ, Verweij MM, Bridts CH, De Clerck LS, et al. Component-resolved diagnosis from latex allergy by microarray. Clin Exp Allergy. 2010;40(2):348-358. Available from: https://doi.org/10.1111/j.1365-2222.2009.03370.x
- Garnier L, Selman L, Rouzaire P, Bouvier M, Roberts O, Berard F, et al. Molecular allergens in the diagnosis of latex allergy. Eur Ann Allergy Clin Immunol. 2012;44(2):73-79. Available from: https://pubmed.ncbi.nlm.nih.gov/22768726/
- Global Initiative for Asthma. Global strategy for asthma management and prevention, 2021. Available from: www.ginasthma.org
- Scadding GK, Durham SR, Mirakian R, Jones NS, Leech SC, Farooque S, et al. BSACI guidelines for the management of allergic and non-allergic rhinitis. Clin Exp Allergy. 2008;38:19-42. Available from: https://doi.org/10.1111/j.1365-2222.2007.02888.x
- Asher MI, Montefort S, Bjorksten B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733-734. Available from: https://doi.org/10.1016/s0140-6736(06)69283-0
- Anandan C, Nurmatov U, van Schayck OC, Sheikh A. Is the prevalence of asthma declining? A systematic review of epidemiological studies. Allergy. 2010;65:152-167. Available from: https://doi.org/10.1111/j.1398-9995.2009.02244.x
- Kong WJ, Chen JJ, Zheng ZY, Shi QM, Zhou Y. Prevalence of allergic rhinitis in 3-6-year-old children in Wuhan, China. Clin Exp Allergy. 2009;39:869-874. Available from: https://doi.org/10.1111/j.1365-2222.2009.03206.x
- Agodokpessi G, Ade G, Dovoedo N, Ade S, Wachinou AP, Fayomi B, et al. Sensitization profile to airborne allergens of patients followed for asthma in Cotonou, Benin: a cross-sectional study using prick tests. Rev Mal Respir. 2015;32(9):930-935. Available from: https://doi.org/10.1016/j.rmr.2014.09.008
- Ngom Abdou KS, Koffi N, Blessey M, Aka Danguy E, Meless T. French Journal of Allergology and Clinical Immunology. 1999;39(7):539-545.
- West RW, Sharip A. Latex anaphylaxis caused by occupational exposure to balloons. Cureus. 2022;14(6). Available from: https://doi.org/10.7759/cureus.25875
- Loverre T, Casella R, Miniello A, Di Bona D, Nettis E. Latex allergy: from discovery to component-resolved diagnosis. 2024;24(5):541-548. Available from: https://doi.org/10.2174/1871530323666230901102131
- Ben Ameur S, Belhadj R, Yaich S, Maaloul I, Damak J, Kammoun T. Medical Tunisia. 2021;99(12):1174-1179.
- Boussetta KBA, Harzallah H, Zouari B, Sammoud A, Bousnina S. Asthma in infants: medium-term outcomes and predictive factors of symptom persistence in preschool age. Rev Fr Allergol Immunol. 2001:565-570.
- Vanker A, Gie RP, Zar HJ. The association between environmental tobacco smoke exposure and childhood respiratory disease: a review. Expert Rev Respir Med. 2017;11:661-673. Available from: https://doi.org/10.1080/17476348.2017.1338949
- Rogliani P, Sforza M, Calzetta L. The impact of comorbidities on severe asthma. Curr Opin Pulm Med. 2020;26(1):47-55. Available from: https://doi.org/10.1097/mcp.0000000000000640
- Turki S, Jbali S, Hachicha A, Chouchane H, Sifaoui A, Charfi MR. La Tunisie médicale. 2024;102(5):303-309.
- Rubner FJ, Jackson DJ, Evans MD, Gangnon RE, Tisler CJ, Pappas TE, et al. Early life rhinovirus wheezing, allergic sensitization, and asthma risk in adolescence. J Allergy Clin Immunol. 2017;139:501-507. Available from: https://doi.org/10.1016/j.jaci.2016.03.049
- Maciag MC, Phipatanakul W. Update on indoor allergens and their impact on pediatric asthma. Ann Allergy Asthma Immunol. 2022 Jun;128(6):652-658. Available from: https://doi.org/10.1016%2Fj.anai.2022.02.009
- Fish JE. Occupational asthma and rhinoconjunctivitis induced by natural rubber latex exposure. J Allergy Clin Immunol. 2002;110(2 Suppl)–81. Available from:https://doi.org/10.1067/mai.2002.125331
- Kelly KJ, Sussman G. Latex allergy: where are we now and how did we get there? Internet J Allergy Clin Immunol Pract. 2017;5(5):1212-1216. Available from: https://doi.org/10.1016/j.jaip.2017.05.029
- Decree No. 2013-327 of May 22, 2013 prohibiting the production, importation, marketing, possession and use of plastic bags in Côte d'Ivoire. Available from: https://www.fao.org/faolex/results/details/fr/c/LEX-FAOC132141/